FIGHTING MALARIA

Anopheles gambiae mosquito feeding Scientists want a multi-pronged approach to be used to combat malaria, which includes malaria mosquito eradication, prevention measures like mosquito nets and drug treatments for those with the disease. The main eradication strategy is to throw every known malaria-fighting method at the disease. Health officials say if all tools — such as nets, medicines and DDT — are utilized the number of malaria cases could be reduced by 90 percent.
Important factors in controlling malaria include: 1) the availability of health services: 2) effectively using prevention strategies; 3) effectively using treatment strategies; 4) availability of effective medicines: 5) an effective health surveillance system; 6) limiting climate change; and 7) availability of good housing.
In July 2008 the U.S. government pledged to spend $48 billion over the next five years to help treat and prevent AIDS, tuberculosis and malaria, with $39 billion to be spent on AIDS, $5 billion on tuberculosis and $4 billion on malaria. Around the same time $3 billion drive to eradicate malaria deaths to near zero was launched in 2008. Among those that supported it are Colgate, Bono, the creator of “American Idol” and the heads of state of several countries.
Some African countries have seen dramatic reductions in malaria rates by employing a number of control techniques.. Malaria deaths were cut by about 50 percent in nine African countries between 2006 and 2008, according to the World Health Organization, including Tanzania, Zambia, Ethiopia, Rwanda and Ghana. But there were still 243 million cases of malaria worldwide in 2008 and 863,000 deaths, mostly among children — with Africa accounting for 90 percent of malaria deaths. [Source: Robyn Dixon, Los Angeles Times, August 14, 2011]
See Separate Articles:VECTOR-BORNE DISEASES CAUSED BY MOSQUITOES, TICKS AND FLIES factsanddetails.com; MOSQUITOES factsanddetails.com DENGUE FEVER factsanddetails.com; MALARIA: ITS HISTORY, PARASITE AND ITS LIFE-CYCLE factsanddetails.com; ARTEMISININ AND MALARIA MEDICINES, TREATMENTS AND DRUGS factsanddetails.com; MALARIA ERADICATION AND DDT factsanddetails.com
Websites and Resources Centers for Disease Control and Prevention (CDC) cdc.gov/DiseasesConditions ; World Health Organization (WHO) fact sheets who.int/news-room/fact-sheets ; National Institute of Health (NIH) Library Medline Plus medlineplus/healthtopics ; Merck Manuals (detailed info many diseases) merckmanuals.com/professional/index ; Global Fund to Fight AIDS, TB and Malaria theglobalfund.org Book: “The Fever: How Malaria Has Ruled Humankind for 500,000 years” by Sonia Shah (2010, Sarah Crichton Books, Farrar, Straus & Giroux).
Obstacles to Combating Malaria

In 2010, the World Health Organization (WHO) said world could stop malaria deaths by 2015 if massive investment is made to ramp up control measures, including wider use of insecticide-treated mosquito nets. The goal was not reached Andrea Crisanti, a molecular biologist at Imperial College London, told the Los Angeles Times:If you have enough money, with sustained effort, you can eradicate malaria. In the United States and in Europe, malaria was eradicated. Unfortunately, developing countries don't have the resources to sustain the use of insecticides over long periods of time and different locations. It requires complex logistics, a lot of money, effort and motivation, and a strong political will. [Source: Amina Khan, Los Angeles Times, April 29, 2011]
It has been said the goal of wiping out malaria is an economic issue rather than a scientific one. A 2020 WHO report said control measures are protecting more Africans against the disease, although three countries — Rwanda, Sao Tome and Principe and Zambia — reported resurgences in the number of cases, illustrating the fragility of gains. Between 2007 and 2010 enough insecticide-treated mosquito nets have been provided to protect 578 million of the estimated 700 million people at risk of malaria in sub-Saharan Africa. A further 75 million are protected by indoor spraying. But funding, estimated at $1.8 billion a year, falls far short of the $6 billion needed to fully control malaria."Current strategies work," said WHO director-general Margaret Chan, calling for continued investment and vigilance. [Source: Stephanie Nebehay, Reuters, December 14, 2010]
Some have argued that one thing that has helped malaria thrive in the developing world is the fact that it has been wiped out in the developed world. Poverty expert Jeffrey Sachs of the Earth Institute of Columbia University has estimated it cost about $4.50 to provide mosquito nets and artemisinin-based drugs for all Africans at risk of malaria, with a total cost of $3 billion necessary to meet the needs of the entire African continent. This is a lot of money for Africa but not that much for the developed world , where $24 billion is paid out in Wall Street Christmas bonuses and millions forked out each day for a $4 Starbucks coffee.
Methods for Combating Malaria

SMS_for Life Methods of combating malaria in areas where the disease is common include: 1) systematically eliminating standing water, where mosquitos breed; 2) spraying houses with insecticide; 3) providing people with mosquito netting; and 4) providing people with drugs that prevent and treat the disease. While many remedies seem simple and cheap by the standards of the developed world they are still expensive and beyond the reach of many in the developing world.
Methods that have been employed in places where malaria has nearly been eradicated have included: 1) applying insecticides to the inside walls of homes every six months; 2) collecting family medical histories and GPS data on handheld devises; 3) simplifying treatment by packaging drugs for individual use; 4) setting up mosquito traps and testing the mosquitos for malaria; 5) using the new finger-stick tests to quickly detect who is sick; and 6) getting the sick on artemisinin-based combination therapy quickly.
The easiest way to avoid malaria is to avoid places with the disease and take measures to prevent from being bitten by malaria-carrying mosquitos, which strike primarily in the evening or at night. People who live in areas where malaria is endemic use mosquito netting (preferable treated with insecticide); have screens on their windows; use insect repellent and light mosquito coils in the evenings.
Spaying the insides of houses, particularly with DDT, has proven to be a very effective malaria-fighting measure. Again since malaria mosquitos bite mainly at night spraying the inside of houses where people sleep reduces he chance of getting bitten, Studies have shown that if 80 percent of the houses in a village or neighborhood almost no one gets malaria. Spraying works because people who are bitten are bitten by mosquitos that have not bitten an infected person and thus don’t carry malaria.
Malaria and Mosquito Nets
Insecticide-treated mosquito nets are amazingly effective in preventing malaria. They can cut malaria infections by half and child deaths by a third. Studies by the U.S. Center for Disease Control and Prevention indicate that widespread use can reduce transmission by 90 percent.
Insecticide-treated mosquito nets are cheap and easy to use. They cost $5 or less. The cost to manufacture, ship and distribute them is about $10 a piece. They are now cleverly engineered so they can last for five years.

distribution of malaria nets in Niger To work mosquito nets need to be installed properly, used regularly and treated every six months to a year with insecticide. The insecticide is more important protecting people from bites than the netting itself. It works by killing mosquitos attracted to the net by the carbon dioxide exhaled from the sleeping people. Not only do treated nets prevent people from getting infected, they reduce the severity of the disease among those who get infected (they have fewer parasites in their blood and less severe fevers).
Nets have been used for some time. Herodotus described Egyptians who wrapped themselves in fishing nets. Nineteenth century British colonists used them in India even before they knew malaria was caused by mosquitos.
About 25 percent of childhood malaria cases could be prevented immediately if children in infected areas used insecticide-treated mosquitos nets. In some parts of Africa mortality rates for children have been reduced by 60 percent by using nets.
Research has shown that people don’t even have to sleep under nets to receive their benefits. A study in Kenya, found that children who didn’t sleep under nets themselves but lived within 300 meters of houses with nets had fewer parasites in their blood and low mortality rates than those who lived in areas with no nets. A study in Ghana showed that mortality rates among children decreased 7 percent every hundred meters closer they lived to houses with nets.
Malaria Net Activism and Entrepreneurship
Millions of dollars has been spent by international agencies, NGOs and USAID on getting mosquito nets into the hands of people that need them. As of 2007 a group called Nothing But Nets had raised $13 million mainly from young people through web-based marketing and used the money to purchase pesticide-treated mosquitos nets for people who need in the developing world.
The Danish company Vestergaard Frandsen S.A. is the world’s largest producer of insecticide-imbedded mosquito nets. More than 48 million Permanets produced by the company were sold in 2007. The company also makes malaria-fighting, insecticide-coated sheeting (ZeroFly) and has developed a trap for tsetse flies.
Groups involved in handing out malaria nets in high-risk areas and educating people about their use include Against Malaria ( www.againstmalaria.com/netdelivery ); Center for Disease Control Foundation (www.cdcfoundation.org/bednets ); Population Serves International (www.psi.org/malaria ); Malaria No More ( www.malarianomore.org ) ; Nothing But Nets: ( www.nothingbutnets.org )
In April 2010, in honor of World Malaria Day, viewers of “American Idol “ were urged to donate $10 for an insecticide-treated bed net to save an African child from malaria.
Distribution and Use of Mosquito Nets

distribution of malaria nets in Niger Mosquito nets require little infrastructure to distribute. A single volunteer on a motorcycle can give out hundreds of them a day even in the most remote areas, There is no need for refrigerators to keep medicines and vaccines cold. Doctors are not needed to set proper doses. Red Cross volunteers have been quite effective in setting up distribution networks and training villagers in Togo and Niger, where more than half of all households in both countries received nets in a matter of a few days.
Charging net users appears to be a better strategy than giving them out free, presumably because more value is attached to them. In his book “The White Man’s Burden: Why the West’s Efforts to Aid the Rest Have Done So Much Ill and So Little Good” (Penguin Press), William Easterly describes how when malaria-fighting mosquito nets are given out free “nets are often diverted to the black market...or wind up being used as fishing nets or wedding veils.” When they were sold for $5 a piece in program in Malawi “the nationwide average of children under 5 sleeping under nets” increased “from 8 percent in 2000 to 55 percent in 2004...A follow up survey found nearly universal use of the nets by those who paid for them” while in a Zambian program that handed out nets free “70 percent of the recipients didn’t use” them.
Problems with Using Mosquito Nets
Despite their obvious benefits mosquito nets are still not widely used. As of 2007, only two percent of children in Africa used them. Many people don’t use them because they don’t like them or find them inconvenient. Even at only $5 a pop for many poor families they are still too expensive. Upkeep is also a problem. Reapplication of pyrethrid insecticide is recommended at intervals of 6 to 12 months with older nets, something many villagers don’t have the time or know-how to do.
Many people don’t like to lie under the nets because they are hot or stop using them when the rainy season ends. A tear in the net or a gap or leg hanging out can allow mosquitoes to reach the body.
The tight mesh that keeps mosquitos out also blocks ventilation and makes the nets hot and uncomfortable. Because they are viewed as hassle and malaria is not necessarily considered a serious ailment people didn’t use them. On top of that people believe that malaria is caused by things such as magic or hard work. Some villagers put the nets above their beds but never unwrap them.
Data indicates that in places where Africans have access to mosquito nets half refuse to sleep under them. Even those that use them don’t necessarily use every night over periods of years. Even the best nets wear out after four or five years. After that time will replacements arrive at the villages? Will villagers have to buy them themselves?
Better technology and more money from donor nations are expected to help rectify the situation. Several companies now produce nets with insecticide imbedded in the fibers of the nets that last for five years and don’t need to be sprayed.

mosquito net
Malaria Research
Scientists have figured out the gene sequence for both the most deadly malaria parasite and the mosquito that carries it. Using this knowledge scientists are working on drugs, vaccines and treatment that attack each stage of the infection: the blood stage, liver stage and even stages in which the falciparum is still in the mosquito.
Researchers from Imperial College London sterilized male mosquitoes by genetically modifying them to neutralize a gene required for sperm production. They argue that releasing genetically modified, spermless male mosquitoes into the wild could in future help and could prevent malaria transmission and reduce the chances of large outbreak. Reuters reported: In a study to see how these mosquitoes would fare when trying to get a mate, they found that female mosquitoes cannot tell if the males they mate with are fertile, or spermless and therefore unable to fertilize the females' eggs.[Source: Kate Kelland, Reuters, August 8, 2011]
Johns Hopkins University microbiologist George Dimopoulos discovered that a class of Enterobacter bacteria living inside the guts of some Zambian mosquitoes makes the insects resistant to Plasmodium falciparum, a parasite that causes malaria. Discover magazine reported: When the two microbes squared off in a petri dish, the gut bacteria could almost totally prevent Plasmodium from growing. Mosquitoes that sucked up both the bacteria and the parasite were unable to transmit malaria. Dimopoulos found that the bacteria unleash a torrent of unstable oxygen molecules that inhibit Plasmodium’s development. Those molecules, he believes, are either natural waste products or chemical weapons that are normally used against rival bacteria. The fact that they kill Plasmodium is a happy accident, and one that Dimopoulos wants to exploit. “The idea is to feed mosquitoes in the field with an artificial nectar supplemented with the bacterium,” he says. “It would be like a probiotic for the mosquito.” [Source: Ed Yong, Discover magazine, January-February 2012]
Scientist are studying female bed bugs as they are the only known creature in the animal kingdom to possess an immune organ, which in turn is being studied as a way of producing a strong immune response of fight disease. The organ produces a wave of white blood cells as a line of defense against sexually-transmitted infections caused by male bed begs that have a needle-like penis that they stab directly into the female’s abdomen rather than insert in the female’s genitals, causing nasty wounds that easily become infected.
Using Smoke and Smelly Socks to Fight Malaria Mosquitoes
Robyn Dixon wrote in the Los Angeles Times: As a boy in remote western Kenya, Fredros Okumu sat under the stars, smothered by the smoke of the family fire, until it was time to go to bed. Even now, when he returns home to his village, a 29-year-old man who left and achieved things, he still sits in the darkness, eyes stinging, nose running, enveloped in the choking smoke. Its smell clings to his hair and clothing, but at least it serves its purpose: keeping the mosquitoes at bay. Like almost everyone in the village of Uyoma, Okumu lost family and friends to mosquito-borne malaria when he was growing up. So the smoke of burning Kenyan bush herbs was his friend. "One of the things growing up, I caught malaria at least twice a year. I lost cousins, around five of them. And if you speak to any African boy who is 29 years old and grew up in an African village, he would either have a similar situation, or worse," he said from Tanzania, where he works as an entomologist for the Ifakara Health Institute, a medical and public health research institute. [Source: Robyn Dixon, Los Angeles Times, August 14, 2011]

Having grown up in a village, Okumu knows what might work, and what won't. "I still visit my village a lot and I see how things are being done," he said. "I still sit around my mother's fire and my nose still runs the way it did 20 years ago and my eyes still sting. Life is not very different." After his mentor, Dutch medical entomologist Bart Knols, discovered the insects' strange affinity to foot odor by standing naked in a room full of mosquitoes to see where they bit him, Okumu was driven to find a cheap, practical way to use the knowledge. His plan would enlist the services of villagers who would wear cotton pads in their socks, to be used as bait in mosquito traps, a cheaper option for villages than using chemically synthesized foot odor.
The project, which has received $775,000 in funding from the Bill & Melinda Gates Foundation and Grand Challenges Canada, is designed to eradicate mosquitoes outdoors, to complement the big strides made in cutting malaria deaths using treated bed nets, malarial drugs and spraying. "We believe African innovators are best placed to solve African problems," said Peter Singer of Grand Challenges Canada, which seeks out African inventors with out-of-the box ideas. "I think there's a lot of value at the table in terms of tapping bright young African innovators who have great ideas and who could be more fully enabled to tackle their own challenges."
It was Knols who discovered that mosquitoes were most attracted to smelly feet. But Okumu decided to apply the discovery to an outdoor mosquito trap. Okumu's plan to use actual smelly socks odor offers a cheap alternative to a chemical smell and can be easily replaced by villagers. He plans to focus on youths playing soccer, or laborers, as a source for the sock pads. "We hope this will reduce the cost but also create a level of interest in the community," he said.
The mosquito trap is a square wooden box with louver vents and a battery-run fan to blow the sock odor into the air through a bamboo pipe. Inside the insects become contaminated with poisons and ultimately die. Experiments were done in three villages in the early 2010s where people get about 350 bites a year from malaria-infected mosquitoes. David Brown wrote in the Washington Post: The traps look a little like commercial beehives. Some contain the human-odor bait, which consists of simple chemicals (including lactic acid, ammonia and propionic acid) that are exuded by people, especially from the legs and feet. Some contain socks worn for a day by adults. Others contain cotton pads that schoolchildren will put inside their socks for a day and then deliver to researchers. The researchers compare the number of mosquitoes caught with each method. [Source: David Brown, Washington Post, July 12, 2011]
Earlier work by Okumu and his colleagues at the Ifakara Health Institute in Tanzania showed that the chemical bait attracted four times as many mosquitoes as live people and that dirty socks worked just as well, at least in the lab. If the sock pads prove adequate, they will be the preferred bait. The inside surfaces of some traps are coated with an organophosphate pesticide. Mosquitoes that land there will die within 24 hours. Other traps contain a fungus that infects the insects and kills them in five days — roughly half the time needed for the complicated cycle that enables a newly infected mosquito to transmit the malaria parasite to a person.
Combating Malaria with DNA Engineering

anemia and malaria In 2011, a team of scientists from Imperial College London and the University of Washington in Seattle reported in the journal Nature on a genetic approach in which mosquitoes were inserted with a fungus gene that attacked specific mosquito genes — making it possible to destroy genes that allow the malaria parasite to reach humans' bloodstreams. [Source: Amina Khan, Los Angeles Times, April 29, 2011]
Andrea Crisanti, the paper's senior author and a molecular biologist at Imperial College London, told the Los Angeles Times: We thought if we developed genetically modified mosquitoes that are unable to transmit malaria — and are able themselves to transmit this genetic modification to local mosquitoes, through mating — that would be an effective solution.
it's a sort of cut-and-paste-function: You have a gene able to attack the other gene, destroy it and copy itself in its location. The technology is based on a gene that makes an enzyme that selectively recognizes DNA sequences and cuts them. Now if you induce a cut in the DNA, a break in the DNA, you trigger the cell's repair mechanism. The repair mechanism then uses the enzyme's gene as a template to repair the broken DNA sequence. And so, key genes in the mosquito that are involved in malaria transmission can be disrupted. As the mosquitoes breed, it spreads through the population.
In the lab, we saw the mutation spread to more than half the population of mosquitoes we had living in cages. This happened in a time span of 12 to 16 generations of mosquitoes (each generation being between 18 to 30 days in the wild). So it's quite efficient. You could, for example, destroy genes that are important for the parasite. There are some genes that are important for the mosquito to recognize and bite humans rather than animals. Or you could destroy genes that regulate sex development for female mosquitoes, so every generation will produce only males. This will, in the span of a few generations, have tremendous impact on the size of the mosquito population.
See Separate Article MOSQUITOES: BLOOD, DISEASE AND AVOIDING AND KILLING THEM factsanddetails.com
People with Resistance to Malaria
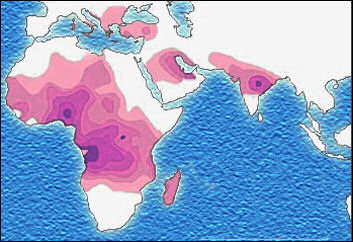
Sickle cell distribution Why do some people who don’t take a prophylactic in malaria-infested area get malaria and others don't? Sometimes people simply avoid getting bitten by malaria-carrying mosquitos. Sometimes they actually have the disease but show few symptoms. Other times they have built up a resistance to the disease.
In some malaria-endemic areas in Africa people have not built up an immunity to the disease, but their bodies have learned to live with it. In Kenya about 40 percent of adult have the parasites in their blood. In some villages in Kenya and Tanzania, all the children tested have the malaria parasite in their blood. Sometimes they don’t appear sick but have so many parasites in their blood that if they were given a blood test on the United States they would be rushed to an emergency room.
Children who survive bouts with malaria usually develop immunity to disease that allows them to survive with the disease in their blood and display few symptoms other than increased fatigue when the get the disease later in life. When they are rid of the disease they say they feel better than they ever have before — in other words, normal.
In some places in Africa, people average 200 infectious bites from malaria-carrying mosquitos a year and get an average of 43 bouts of malaria in their lifetimes. Because of their tolerance to the disease. they often fare better than people who get 10 infectious bites a year and contract malaria 62 times in their lifetime, Bearing this in mind, some doctors believe that people would probably be better served if they didn't use mosquito nets or preventative medicine and were let to build up natural tolerance to the disease.
Malaria Immunity
Over the past 10,000 years several mutations have been “naturally selected” to protect humans from malaria. Behind the changes is the Darwinian concept that any mutation that protects a victim from an early death will allow them to reproduce and spread the mutation. Africans have developed a number of genetic mutations that protect them against malaria that became widespread even though they also caused also sickle cell anemia, thalassemia and G6PD deficiency. Mutations that fight the disease have also been found in Thailand and New Guinea, where malaria is also prevalent.
People with a disease called alpha thalassemia — a genetic blood disorder found in the tropics that produces abnormally small red blood cells, often rendering victims listless with mild anemia — offers some protection against malaria. Scientists think the disease protect people against malaria because the malaria parasites destroy a smaller number of their blood cells.
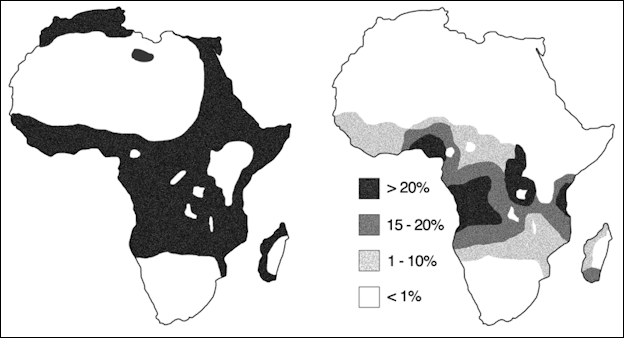
Malaria versus sickle-cell trait distributions
Resistance to Malaria and Sickle-Cell Anemia
In 1948, British biochemist J.B.S. Haldane noticed that the distribution of populations with abnormal hemoglobin coincided with the distribution of malaria. He theorized that genes associated with the abnormal hemoglobin protected those who possessed them against malaria. Sickle cell anemia and hemoglobin C, a variant found in Africa that offers protection against the malaria parasite, and hemoglobin E, a variant found in Southeast Asia that lessens the severity of malaria, indicate that Haldane was largely correct.
People with the blood diseases like sickle-cell anemia, thalassemia, G6PD deficiency and hereditary ovalocytosis are less likely like to get malaria and severe malaria symptoms than people who don't have these diseases because the diseases inhibit the ability of the malaria-carrying protozoans to disrupt red blood cells.
One reason that the sickle cell trait (and the blood diseases listed above) is more common among blacks than among whites is that the ancestors of most blacks lived in malaria-endemic areas, where sickle-shaped hemoglobin prevented people from dying of malaria. Through natural selection the sickle-cell trait was passed down from generation to generation even in places where malaria is no longer prevalent.
Onge and Malaria
The Onge of India’s Andaman Islands have a sickle-shaped cell keeps which helps prevent them from getting malaria. Some Africans and black have similar cells which help fight off the disease. Andaman Islanders use an herbal brew that some biologist say might be a cure for malaria. Microbiologist Debaprasad Chattopadhyay made the discovery that the Onge had seemed to have found a cure for malaria but the Indian government has refused to publish the formula to protect the tribe and keep it being exploited by profiteering drug companies.
Chattopadhyay lived with the Onge in one of their beehive-shaped huts and found that even though the Onge were surrounded by malaria-carrying mosquitos they didn't come down with the disease. He was given several plants used to make the potion. In his laboratory in the Andaman town of Port Blair he discovered two of the plants contained anti-fever properties and a third reduced the number of malaria parasites in infected humans. Chattopadhyay himself came down with malaria. When he took the potion he was cured in three days. Since then his malaria has not reoccurred. He also gave the mixture to some local doctors. All seven of the patents who took it were cured as well.
Malaria Vaccines

As of 2007, 90 teams around the world were working on some aspect of a malaria vaccine. As an incentive, the British government has pledged to purchases hundreds of million of doses of any successful vaccine for donations to countries that need it.
As it stands now vaccines have been developed that successfully fight bacteria and viruses but none have been conceived that prevent parasitic diseases. Making the goal of creating a malaria vaccine even harder to attain, is the fact that the malaria parasite is very complex. It has over 5,000 genes, compared to just 11 for the polio virus, and its development cycle makes it a difficult-to-hit moving target.
If a promising vaccine is developed it has to be totally successful. A partially successful one could be worse than nothing, allowing the malaria parasite to develop resistance and make it more difficult than ever to combat. On top of that each type of parasites has it numerous substrains and a vaccine has to be effective on them all.
Among the vaccine strategies that hold the greatest promise are: 1) blocking development of the parasite in the mosquito; 2) blocking the parasite from entering the liver or growing inside it; and 3) preventing invasion of the red blood cells or reducing the severity of the infection. One goal among researchers is to create a vaccine that works on young children, who are most vulnerable to the disease.
In October 2008, the Gates Foundation said that it would donate $168 million to develop a malaria vaccine.
Difficulty in Making a Malaria Vaccine
Producing an effective malaria vaccine is a major goal of modern medicine. But is no easy task. No one has ever created a vaccine that works against a parasite, although decades have been spent trying. Many substance have been found that kill the malaria parasite but so far none have been found that kill it without harming the humans who take it.
As is true with AIDS and tuberculosis, malaria does not elicit a full response by the human immunity system. Morever, the malaria-causing protozoa has a lot more genetic material and is much more complex than a virus or bacteria. As a result it is difficult to develop a vaccine against the disease. and people are less likely to build up immunity to it than to other diseases.
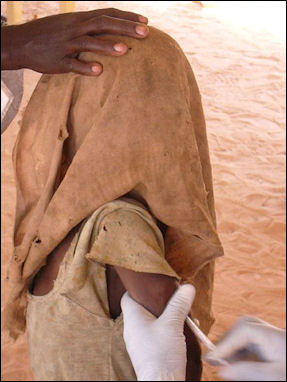
Being vaccinated for other
diseases in Chad Explaining how this is possible, malaria researcher Dr. Stephen Hoffman told Smithsonian, "First of all, Phasmidia have about 6,000 genes in their DNA, compared to viruses like smallpox or measles, which have less than 30. The organism has built-in redundancy, so it can more readily escape attack. Second if you take, say, a 6-year-old child from sub-Saharan Africa who has malaria, he may have as many as five different strains existing at once within him. And you have to have a vaccine that attacks all five. Lastly, the parasite matures and circulates in different forms in the human body, hiding inside existing cells until it's ready to attack. So you have to create multiple vaccines, in effect, that are each stage-specific, and then combine them."
Another obstacles that has be overcome is expense: the vaccine has to be cheap if it is going to be widely used where it is needed in the developing world.
Efforts to Make a Malaria Vaccine
A malaria vaccine, known as SPf66, was developed in 1988 by Columbian biochemist Manuale Patarroyo, who heralded his discovery as a “cure” for malaria and formally donated it to the WHO. Given in a series of three injections over six months and tested on thousands of people, the vaccine does not prevent malaria but reduces the chance of getting it. In a test in Tanzanian village where virtually everyone is infected by the parasite by the age of 5, children given the vaccine had 31 percent fewer cases of malaria than those who didn’t. Field tests in Gambia and Thailand, were the toughest strains of malaria exist, have been less promising. In some cases people who took the vaccine were more likely to get malaria than those who didn't.
A malaria vaccine called MSP/RESA, or Combination B, appears to reduce the severity of some malaria infections . It is most effective against the “plasmodium parasite falciparum” found in Papua new Guinea.
In Europe, scientists are experimenting with using mosquitos to deliver a “vaccine” of live malaria through their bites. In a study performed at Radboud University in Nijmegen, Netherlands, a group that underwent the “treatment” didn’t catch malaria when exposed to the disease whereas all members of group that didn’t receive the treatment did come down malaria.
In a study published in the New England Journal of Medicine in August 2009, 10 volunteers in a “vaccine” group and five others in a comparison group were given chloroquine for three months. The “vaccine” was exposed to about a dozen malaria-infected mosquitos. The “comparison” group was exposed to non-infected mosquitos. Then all 15 stopped taking chloroquine. Two months later they were all exposed to malaria-carrying mosquitoes. None of the 10 volunteers in the “vaccine” group caught the disease while all five in the comparison group did. Researchers were careful to point out the method was not a real vaccine and was not practical in a large group but it did show the possibilities of working with live malaria parasites to combat malaria.
Another promising vaccine has been developed by a team lead by W. Ripley Ballou at the Walter Reed Army Institute of Research.
Sanaria Malaria Vaccine
malaria in the U.S. in the 1920s Dr. Stephen Hoffman heads Sanaria — which means “healthy air,” the opposite of malaria — the only company in the world dedicated to finding a malaria vaccine. Hoffman served 14 years as head of the malaria program at the Naval Medical Research Center and was once so confident that he found a vaccine he tested it on himself and exposed himself to infected mosquitos, only to come down with the disease hours before he was going to announce his great discovery at a medical conference.
Sanaria operates out of an office in a mini-mall in a Maryland suburb outside Washington D.C. Infected mosquitos are kept in an areas that is secured by sealed doors that look sort of those on the international space station. The vaccine that shows the most promise is one that consists of irradiated parasites produced by exposing infected mosquitos to high doses or radiation. The technique builds on work done by the late Ruth Nussensweug of New York University, who found that radiation-weakened mosquitoes prompt an immune response in mice without causing malaria. Field studies were scheduled to being in 2008.
Vaccines made with sporozoites that have been weakened by radiation so they can not cause harm have showed promise. Getting the amount of radiation right is tricky. The sporoziotes have to be weakened enough so they do not cause malaria but strong enough to trick the immune system into protecting the body from the disease.
RTS,S Vaccine

Blood collecting safari, 1953 An injectable vaccine called RTS,S produced by GlaxoSmithKline has been shown to offer partial protection. In a study with 2,000 children in Mozambique completed in 2004 the drug reduced the chance of getting malaria by a third and reduced the chances of developing severe malaria by 58 percent for more than a year. Data released in 2008 said it reduced the risk by 53 percent for children between 5 months and 17 months and was shown to be safe when given with other vaccines.
RTS,S, also known as Mosquirix, is the first potential malaria vaccine that has gotten as far as large scale safety trials. It is also the first vaccine to target a more complex human parasite than a bacterium or virus. Although the data thus far shows the vaccine is far from perfect even a partially effective vaccine has the potential of saving hundreds of thousands of lives.
In May 2009, a large clinical phase three trial of the RTS,S treatment began. In the early stages the vaccine was been given to 5,500 children in seven African countries, including Kenya, Tanzania,, Malawi, Mozambique and Gabon. The trial will eventually involved about 11,000 to 12,000 children. Scientist have said the RTS,R trials will be ready by 2012 and the vaccine will be ready for widespread distribution by 2015.
Image Source: Centers for Disease Control and Prevention cdc.gov/DiseasesConditions ; Wikimedia Commons
Text Sources: Centers for Disease Control and Prevention (CDC), U.S. Department of Health and Human Services; World Health Organization (WHO) fact sheets; National Geographic, New York Times, Washington Post, Los Angeles Times, The New Yorker, Time, Reuters, Associated Press, AFP, Lonely Planet Guides and various websites books and other publications.
Last updated May 2022
