DISEASES IN SOUTHEAST ASIA
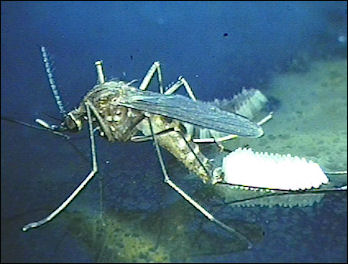
Culex vishui mosquito, source of Japanese Encephalitis Major infectious diseases found in Southeast Asia include bacterial diarrhea, hepatitis, dengue fever, malaria, Japanese encephalitis, rabies, and leptospirosis. Schistosomiasis (bilharziasis) is present in Thailand but the chances of getting it are relatively low. High risk areas include the southern parts of the Mekong River and lakes in northeastern Thailand. There are lots of leeches in the jungle in the wet season bu they generally don't cause any disease.
Liver Flukes occasionally infect people in Laos and northeastern Thailand. They are picked up primarily from eating raw or uncooked fish. Some people get them from eating uncooked “paa daek” (unpasteurized ferment fish used in many Thai foods). See Raw Fish Linked to Liver Cancer in Southeast Asia Below. Japanese Encephalitis occurs particularly in the rainy season. It is said the highest risk areas are around rice fields and places where pigs are raised since pigs and wild birds (that hang out in rice fields) serve as reservoirs for the disease. See Below.
The Asia-Pacific region accounts for a third of global tuberculosis (TB) cases, with China, Cambodia, Vietnam and the Philippines representing 80 percent of the region’s tuberculosis, said the U.N. health body. The WHO estimates tuberculosis is spreading globally at a rate of one person per second. Every year eight to 10 million people contract the disease and two million die, it said. [Source: Reuters, September 23, 2005] See HEALTH ISSUES IN SOUTHEAST ASIA factsanddetails.com
Diabetes in Asia
Diabetes numbers are particularly bad in Asia, where there seems to be a genetic disposition to the disease brought out by development and a more affluent life-style. For a person of European background the risk of the disease rises when the body mass index reaches 26. For Asians it starts at 22 because they put on fat in the abdominal area . That body shape is linked to insulin resistance.
Time reported: The cost is huge. The World Health Organization predicts these diabetes-linked chronic diseases will cost China alone about $558 billion in lost productivity and healthcare costs over the next decade, taking a large bite out of the country's hard-fought economic gains.[Source: Emily Rauhala, Time, June 1, 2009]
Jeremy Laurance wrote in The Independent: “Across the Far East, growing urbanisation, rapid industrialisation and increasing obesity associated with decreased physical activity is fuelling an epidemic that has killed as many as Aids but has received a fraction of the attention. The disease is diabetes, and its incidence is accelerating, leading to an epidemic of amputations and blindness, the two commonest effects of the condition. Developing nations are hardest hit; they bear 90 per cent of the burden but have only 10 per cent of the resources to deal with it. [Source: Jeremy Laurance, The Independent, February 27, 2006]
“The most striking thing about the patients at the Thanh Hoa clinic in Vietnam is how few of them are fat. In the West, obesity is the chief driver of the epidemic — the Royal College of Paediatrics and Child Health has just released a new report showing that soaring levels of obesity among children in the UK are sparking a crisis of diabetes in under-16s. But Mr Can is lean and spry as are most of the other patients. Doctors do not know why Asians are more prone to the disease. One theory is that because of their slighter build, compared with Westerners, they have less muscle bulk and more fat, so do not need to gain much weight to put themselves at risk. Malnourishment in infancy or in the womb, which is known to increase the risk of diabetes, may also play a part. Seven out of 10 of the worst affected nations by the disease are in Asia. India already has a total of 31 million cases, the highest in the world, closely followed by China with 20 million. The Far East is expected to see the fastest growth by 2025, with a near doubling in the current total of 81 million cases to 156 million.
“Becoming blind or losing a limb is a huge problem anywhere but in the developing world it is a disaster. In India, 45,000 amputations are carried out a year because of diabetes, all of them unnecessary with the correct care, according to Anil Kapur, vice-president of the WDF. "We are faced with a diabetes pandemic," Dr Kapur said. But the world only recognised infectious diseases as a threat. Of the $2.9bn (£2bn) given in overseas aid for health in 2002, just 0.1 per cent was allocated to chronic diseases including diabetes, he said.
“The food companies exacerbate the problem with sales techniques such as mini-sizing, according to Gauden Galea, regional adviser for the World Health Organization. Mini-sizing — selling soft drinks and fast foods in miniature portions — is a growing practice in the region. While the food companies argue they are offering customers a low cost option, Dr Galea claims it is a cynical way of boosting their business. "They are sowing a taste for fast food by inveigling their way into people's eating habits. As people become more affluent they move from mini size to super size." But Dr Galea says the global trend towards increasing weight, which is fuelling the pandemic of diabetes, can be halted. Successful public health projects were carried out in Da Qing, China, a decade ago based on intensive education on diet and exercise, which led to a 47 per cent reduction in the incidence of diabetes over six years. Similar projects in the United States, Finland and India achieved comparable results. "These projects demonstrate very conclusively that you can delay or prevent diabetes with only minor reductions in weight," Dr Galea said. The challenge, he added, was to ensure that the care given to Mr Can could be delivered across the Far East.
Dengue Fever

aegypti mosquito, source of dengue fever Dengue fever is a nasty, viral disease transmitted by the “Aedes” mosquito, usually the “ Aedes aegypti” , the same mosquito that often carries yellow fever. Sometimes called "breakbone fever" or "break-heart" because of the intense pain it can produce, the disease is characterized by sudden onset of fever; intense pounding, frontal headaches; aching bones and joints; nausea and vomiting; and a feeling of being too sick to eat anything. Other symptoms include severe sweats, symptoms: eye pain, rash, chills, and excruciating chest pains. Tests foe dengue rely on the presence of antibodies, which can take up to a week to develop.
Dengue fever is found in 100 countries and kills about 20,000 people annually. Nine out of 10 people who get dengue fever don’t even feel it or get a mild case in which they feel something akin to a slight flu. People who get full-blown dengue fever are sick for a week or more. Many patients have a rash, which appears 3 to 5 days after the onset of the disease, and experience severe emotional and mental depression during the recovery period. Most cases of the disease are benign and self-limiting although convalescence may take a long time.
A few people with dengue fever suffer gastrointestinal bleeding. Fewer still suffer brain hemorrhages. In about 1 percent of cases dengue fever can cause a severe and often fatal hemorrhagic disease called dengue hemorrhagic fever (DHF) that occurs when capillaries leak and the circulatory system collapses.. Those that die of dengue fever often get DHF hemorrhaging in the final stage of the sickness. Failing to realize they are infected, they go don’t get treatment soon enough and lose blood plasma and go into shock after the initial fever passes. Some victims die within 10 hours of developing serious symptoms if they don’t get appropriate treatment.
See Separate Article DENGUE FEVER factsanddetails.com
Japanese Encephalitis
Japanese encephalitis is a mosquito-born viral disease that usually infects people in rural areas in the summer and autumn in temperate regions and northern tropical zones of Bangladesh, China, India, Cambodia, Korea, Laos, Myanmar, Nepal, Thailand, Vietnam and eastern Russia. It is sometimes present in the wet season in the tropical zones of south India, Indonesia, Malaysia, the Philippines, Singapore, Sri Lanka. Taiwan and south Thailand.
Japanese encephalitis is transmitted chiefly by the Culex vishui and Culex tritaeniorhyncus mosquitos, which bite mainly in the afternoon and evening and develop from larvae found mainly in cultivated rice fields and marshes. People traveling in rural areas have a stronger likelihood of contacting the disease than those who stay in urban areas.
Japanese encephalitis can cause paralysis, seizures and death. It strikes about 30,000 people a year. It has killed more than 3 million children worldwide since the 1960s. Most people who are infected display no symptoms, but the fatality rate is as high as 30 percent among victims who are hospitalized. Severe swelling in the head and central nervous system are manifestations of severe cases of the disease.
There is a vaccine that is given in a series of two or three injections one or two weeks apart. There is no medical cure but most victims recover on their own with rest and hospital care.

where Japanese encephalitis is found
Malaria in Asia
India, Myanmar, Papua New Guinea and Indonesia are among the Asian countries with the highest numbers of cases and deaths.Malaria is common in some parts of Southeast Asia. Of the 1.1 million people who died of malaria in 1998, 73,000 died in Southeast Asia. On the border of Thailand and Cambodia about 80 percent of the malaria is mefloquine resistant (1994). Preventive measures have lowered the rate among men but the virus is still spreading among women and children. About 6,400 children are infected annually.
Malaria is found in rural areas, but there is generally not much of a risk if you stay close to the cities and the beach resorts. Dangerous chloroquine- and Fansidar-resistant strains of malaria are common, especially near the borders of Thailand, Cambodia and Myanmar . Mefloquine-resistant strains have also been reported. Chloroquine, Fansidar and Mefloquine are the preventative anti-malaria medicines people usually take in malaria areas. Be especially careful in swampy areas and during the monsoon season. Malaria has been “practically eliminated” from coastal areas of Thailand (it is still found on some islands near Cambodia).
The most virulent and drug resistant from of malaria (Falciparum malaria) is found along the Thai-Myanmar border. Untreated the disease is often fatal. The disease has largely been kept under control thanks to doctors, using modern diagnostic method and he Chinese herbal "wonder drug" artesunate in refugee camps in Thailand near the Burmese border. The malaria rate in the camps is 1 to 5 percent compared to 25 percent in border regions in Burma. Unfortunately some doctors have been attacked by Karen guerrillas.
Malaria medication is harmful if it is taken more than several months, consequently local people usually take precautions against being bitten by mosquitos — primarily mosquito netting over their beds and mosquito coils lit in the evenings. Many of the antimalarial medicines sold in Southeast Asia are fake. A study by Lancet in 2001, found that a third of antimalarial drugs sold in Cambodia, Thailand, Vietnam, Laos and Burma contained no active ingredient. Low cost alternatives methods of combating malaria include breeding fish in ponds where mosquito larvae live, filling pits that collect standing water and planting eucalyptus trees in marshy areas.
Urban areas is Asia were one thought to be fairly safe from malaria. But that is no longer always the case. The disease is particularly prevalent around cities in India. Malaria was nearly eradicated in India. The Indian government runs the world's largest anti-malaria campaign. In the 1950s there wee an estimated 75 million cases of malaria a year, with 800,000 fatalities. By 1965, there were only 100,000 cases and considerably less fatalities. Much of the success was due to the use of DDT.
Drug-Resistant Malaria in Southeast Asia
In the monsoon jungles of northern Thailand and forest along the Thai-Cambodia border, malaria has managed to mutate so quickly that every known preventative medicine is either ineffective or partially effective for reasons that are still unknown. Nearly all the people in the stricken area on the Thai-Cambodia border, mostly gems miners, farmers and refugees who fled the Khmer Rogue, came down with malaria in the early 2000s. Many got very sick and more died of the disease than in other places. In Thailand, 15 percent of the deaths at Karen refugee camps in the region are caused by malaria.
Drug-resistant malaria was found on the Thailand-Cambodia border in 2004, and later was discovered along the Thailand-Myanmar border. The story of malaria resistence ges back much futher in Asia. Claire Panosian Dunavan wrote in Discover magazine, “The earliest sightings of chloroquine-resistant parasites date as far back as the late 1950s and early 1960s. Clinical failures first surfaced along the Thailand-Cambodia border, in Colombia’s Magdalena Valley... In the early phases of the Vietnam War, nearly 10 percent of American soldiers came down with malaria; many cases were due to drug-resistant parasites. With their first-line treatment failing, U.S. military doctors quickly moved to mefloquine, a potent replacement. Across the battle lines, Ho Chi Minh, faced with the same problem, appealed for help to then Chinese leader Chou En-lai. His timing couldn’t have been better because it coincided with China’s campaign to reassess plants once used in traditional medicine. That effort turned up the ancient Chinese herb qinghao (artemisinin). [Source: Claire Panosian Dunavan, Discover magazine, August 2005]
“By the late 1980s, some Asian strains were impervious not only to chloroquine but also to sulfadoxine-pyrimethamine, a low-cost alternative to chloroquine, mefloquine, and quinine. Malaria deaths were on the rise. In Vietnam, for example, malaria mortality increased 300 percent between 1987 and 1990. Vietnamese health officials responded with bed nets, community health care, and annual malaria surveys. But their most potent weapon was artesunate. In one southern village, artesunate treatments lowered the proportion of residents with blood parasites from 42 to 4 percent in just five years. And on the Thailand-Myanmar border, using artesunate plus mefloquine stemmed the high rate of malaria infections and restored mefloquine to its previous efficacy.
Drug-Resistant Malaria Spreads Rapidly to Thai-Myanmar Border
In April 2012, AFP reported: “Deadly malaria that is resistant to drug treatment has spread rapidly from Cambodia to the border between Thailand and Myanmar, raising concerns of an uncontrollable epidemic, scientists said. A pair of studies published in The Lancet and the journal Science showed how the disease is moving fast into new territory and identified a region of the parasite's genome that may be responsible for mutating in order to survive. [Source: AFP, April 5, 2012 **]
“Malaria that was resistant to treatment with the current standard therapy, artemisinin, was confirmed in Cambodia in 2006 and has since surged 800 kilometers (500 miles) westward to the Thailand-Myanmar border, the researchers said. By studying 3,202 patients along the northwestern border of Thailand near Myanmar from 2001 and 2010 and measuring the time it took them to clear malaria infections from their blood after treatment, scientists were able to show a steady increase in drug resistance. **
“The number of slow-clearing infections rose from 0.6 percent of cases treated in 2001 to 20 percent in 2010. In western Cambodia, 42 percent of malaria cases were resistant between 2007 and 2010, indicating that the Thailand-Myanmar region was swiftly catching up to Cambodia's rates. "Genetically determined artemisinin resistance in P. falciparum emerged along the Thailand-Myanmar border at least eight years ago and has since increased substantially," said The Lancet study. "At this rate of increase, resistance will reach rates reported in western Cambodia in two to six years." **
“The research in the journal Science focused on what was making these parasites different, and found that a region on chromosome 13 of the parasite was strongly associated with slow clearance of infection. They sequenced the genomes of 91 P. falciparum parasites from Cambodia and western Thailand and compared them to parasites from Laos, where resistance to the latest artemisinin-based drugs has not yet emerged. They found seven genes that may be responsible for making the parasite resistant to drugs, and which may explain up to 35 percent of the growing resistance in southeast Asia. **
"We have now seen the emergence of malaria resistant to our best drugs, and these resistant parasites are not confined to western Cambodia," said leader of the study Francois Nosten, director of the Shoklo Malaria Research Unit that studies and treats malaria in the Thai-Myanmar region. "This is very worrying indeed and suggests that we are in a race against time to control malaria in these regions before drug resistance worsens and develops and spreads further." **
Artemisinin-Resistant Malaria in Southeast Asia
The WHO said in 2010 that a form of malaria resistant to the most powerful drugs available — artemisinin-based combination drugs, known as ACTs — may have emerged along the Thai-Myanmar border and Vietnam. Artemisinin-resistant malaria first broke out along the Thai-Cambodia border in 2006. "Studies published in The Lancet and Science journals in April 2012 reported that artemisin-resistant malaria, was detected on the Thailand-Myanmar border 800 kilometres (500 miles) west of where it was first spotted in Cambodia. If we lose the ACTs, we are back to square one. There are no replacement drugs on the immediate horizon," warned the WHO . [Source: Stephanie Nebehay, Reuters, December 14, 2010]
The World Health Organization said in September 2012 that governments in the Mekong region must act “urgently” to stop the spread of drug-resistant malaria which has emerged in parts of Vietnam and Myanmar. AFP reported: There is growing evidence that the malaria parasite is becoming resistant to a frontline treatment, the anti-malarial drug artemisinin, in southern and central Vietnam and in southeastern Myanmar, the WHO said. Drug-resistant malaria in Vietnam is mainly concentrated in three central and southern provinces, say health officials, adding that there are a number of key factors which make tackling the problem difficult in the communist country. Resistance to artemisinin does not prevent patients being cured, thanks to other partner drugs, but treatment typically takes a few days instead of 24 hours. [Source: Agence France-Presse, September 27, 2012]
WHO regional director, Shin Young-soo, said countries must “urgently address this issue before we put at risk not only the fragile gains we have made in malaria control but also our goal of a malaria-free Western Pacific Region.” Countries in the Mekong region must “intensify and expand” operations to contain and eliminate artemisinin-resistant malaria, Shin said at a WHO regional meeting in Hanoi.
The population in the affected provinces are very poor, highly mobile, and have not widely embraced DEET-treated mosquito nets which could reduce malaria infections, according to media reports of a government conference in July. People in the affected provinces often received outpatient treatment and frequently fail to complete a full course of anti-malarial treatment.
One-Third of Malaria Drugs in Southeast Asia Are Fake
More than a third of malaria drugs examined by scientists in Southeast Asia were fake “These findings are a wake-up call demanding a series of interventions to better define and eliminate both criminal production and poor manufacturing of antimalarial drugs,” Joel Breman of the Fogarty International Center at the US National Institutes of Health (NIH) said. [Source: AFP, May 28, 2012]
AFP reported: Trawling through surveys and published literature, the researchers found that in seven Southeast Asian countries, 36 percent of 1437 samples from five categories of drugs were counterfeit. Additionally, 30 percent of the samples failed a test of their pharmaceutical ingredients.
Many of the drugs that are being faked or poorly manufactured are artemisin derivatives, the study said.This is especially worrying as artemisinins are the frontline treatment for malaria, replacing drugs to which the malaria parasite has become resistant.The study says there are many causes for the problem, ranging from widespread self-prescription of drugs to shoddy controls to monitor drug quality and prosecute counterfeiters. Poor-quality antimalarial drugs are very likely to jeopardise the unprecedented progress and investments in control and elimination of malaria made in the past decade,” said Mr Breman.
Rabies in Asia
Rabies carried by rodents and dogs has been reported in the countryside. In 2001 there was a report of a rabid dog biting 52 people in three-hour rampage in Thailand. Fifty people died from rabies in Thailand in 2000 and 29 died in the first nine months of 2001, according to the Public Health Ministry.
Asia is experiencing a resurgence of rabies. Each year, about 55,000 people around the world die from rabies, more than 80 percent of them in Asia, according to the World Health Organization (WHO). In China, more than 2,400 people die of rabies each year, a sharp climb from less than 200 in 1996. By some estimated there are 17,000 rabies deaths in India each year. Making the virus more tragic is that the victims tend be very young and very poor. Half of all human rabies deaths occur in children under the age of 15, says WHO, and more than 90 percent of human rabies victims in China are low-income farmers living in poor provinces, according to a study published in 2006 in the Chinese Journal of Epidemiology. [Source: Geoffrey Cain, Time, October 12, 2010]
Geoffrey Cain wrote in Time: Dogs, bats, foxes and other warm-blooded mammals carry the virus in their saliva and spread it through bites, scratches or licks on open wounds. People who've been exposed can expect a hellish demise — unless they immediately clean their wounds and seek a post-exposure treatment. Typically between 10 days and a year after exposure, patients can experience headaches, irritation, a fever, insomnia and feel pain or twitching at the location of their bite wound. Two to 10 days after those first signs appear, patients hallucinate, convulse, become paranoid at the sight of water and experience seizures and paralysis before they die typically from respiratory failure. Rabies has the highest fatality rate of any infectious disease, according to Dr. Deborah Briggs, head of the Global Alliance for Rabies Control, a Kansas-based non-profit organization. She says, "Basically when you get it, you die."
Health officials point to a variety of reasons for the surge in rabies. In remote provinces in countries such as China, India and Bangladesh, many rabies infections go undocumented, making it difficult to swiftly pinpoint outbreaks and deliver the necessary post-exposure treatments. Meanwhile, over the past decade public health experts have been fighting urgent outbreaks such as swine flu, bird flu and SARS, overshadowing the gradual rise in the human rabies cases. The fact that poor people are most susceptible to rabies puts initiatives against the virus even further under the radar, says Dr. François-Xavier Meslin, the Geneva-based team leader for neglected zoonotic diseases at the WHO.
Others blame governments for not following through effectively. In the 1990s, some Asian governments blithely assumed they were close to eradicating rabies, leading them to prematurely cut down on much needed prevention and surveillance programs. In China, for example, the number of human rabies cases dropped from about 3,500 in 1990 to 159 six years later, thanks to the government's strict enforcement of domestic dog vaccination and the culling of stray ones. But after the government disbanded most of the country's rabies teams in the mid-1990s, the number of rabies cases predictably shot back up to over 2,000. It's a stark reminder of what can happen when a country doesn't stay on top of disease prevention, even if an epidemic appears to be withering.
The abundance of rabies vaccines for dogs and humans make these deaths completely preventable, Briggs says. Even after someone is bitten, health care workers can quickly inject around the wound a combination of a booster vaccine and rabies immunoglobulin, or antibody. After that, they typically follow up with four more injections every few days for the next month. For the world's poorest people, however, obtaining the vaccine can be prohibitively expensive, and Meslin argues that requires stronger government subsidies in countries such as China and Laos.
Few public health officials advocate the killing of animals unless absolutely necessary, and many Asians are Buddhists or Hindus, which oppose killing animals. With enough support and funding, “locations with a growing rabies problem can hope to repeat the success of Bohol, an island of 1.4 million people in the central Philippines that has witnessed the complete eradication of dog and human rabies. Prior to 2007, the island had one of the highest human rabies death rates in the country, but the government and health care organizations aggressively promoted education and surveillance and vaccinated over 70 percent of dogs according to WHO's guidelines. It shows that governments can curb Asia's growing rabies problem while saving its animals. Says Girardi of BAWA, "We now have a humane alternative for protecting our people and our animals."
See Separate Article SERIOUS DISEASES STILL FOUND IN THE DEVELOPING WORLD factsanddetails.com
Raw Fish Linked to Liver Cancer in Southeast Asia
In 2007, Reuters reported: “Thai researchers have urged people in Southeast Asia to stop eating raw freshwater fish because they risk becoming infected with a parasitic worm that may predispose them to developing liver cancer. At issue are parasitic worms, commonly known as fluke, which infest rivers in rural parts of Thailand, Vietnam, Laos, Cambodia, Korea and China. The worms find their way into freshwater fish, and into humans when the fish is consumed raw. [Source: Reuters, July 9, 2007]
Writing in the latest issue of the Public Library of Science journal PLoS Medicine, the researchers said most people infected with fluke showed no symptoms but some went on to develop liver cancer years later. "Less than 1 percent who are infected with fluke will get liver cancer, but those who get infected are in the millions in Thailand, Cambodia and Vietnam. There are 6 million (infected with fluke) in Thailand," said Banchob Sripa of the pathology department in Thailand's northern Khon Kaen University.
Banchob has studied the link between fluke infection and liver cancer, particularly in the bile duct, for more than 20 years. He and his colleagues found fluke infection to be especially serious in the north and northeastern provinces of Thailand, where a raw fish dish, called Koi-Pla, is popular. "Stop eating this, it's the easiest thing to do," Banchob said. He said fluke attack the human bile duct and the incursion triggers a "cytokine storm" — an immune response so intense that it destroys not only the parasites, but the person's surrounding tissues as well.
"There are two mechanisms. The fluke has two suckers. It can bite the surface epithelium of the bile duct and cause ulcers. The second is the inflammation," Banchob said. "The ones with more inflammatory cytokines may have more inflammation ... and these may develop cancer later on." Liver cancer is usually diagnosed when it is far advanced because symptoms surface late. "Most who are diagnosed have advanced cancers, like stage 4, so they only get palliative care. It is very difficult to detect early lesions because there are no symptoms," he said. Most deaths occur within six months to a year of diagnosis. "There would be zero survivors after five years," he said.
Swine Flu in Asia in 2009
In April 2009, Reuters reported: “Across Asia, people are closely following the global spread of swine flu from Mexico and preparing for the worst after the World Health Organisation raised its alert level for the outbreak. Authorities in the region have boosted surveillance at airports and hospitals, stockpiled anti-viral drugs and other supplies to fight any outbreaks. Face masks and anti-viral drugs like Relenza and Tamiflu flew off the shelves from pharmacies in some cities.
"It's really apparent, people have been buying face masks all day," said Cyrus Chan, the boss of a dispensary in Hong Kong's Wanchai bar district who had sold out his entire stock of 10,000 adult face-masks and only had child sizes left. "Since SARS, this is the second time there's been such a great demand," Chan added, as a steady stream of customers asking for masks were told there wouldn't be any new stocks of adult masks till later. Still, the mood on the streets appeared largely calm, with the world's most populous region, used to outbreaks of SARS and the H5N1 avian flu, not having yet reported any confirmed cases. [Source: Reuters, April 28, 2009]
“In South Korea, health authorities are testing a 51-year-old woman for suspected swine flu after a trip to Mexico. "There hasn't been much of a reaction yet. I've just had a few calls asking if we have anti-viral drugs or special masks" said a pharmacist in downtown Seoul. "I guess South Koreans have grown accustomed to these breakouts over the past 10 years. But I will be bringing in more Tamiflu to the shelves."
“Asia's patchy medical infrastructure, poverty and vast populations in countries like China and India make it particularly vulnerable should the virus take hold and propagate. China has vowed to disclose any human cases of swine fever promptly, while state-run newspapers on Tuesday urged officials to be open and avoid the kind of cover-ups that brought panic during the SARS epidemic.
“In Singapore, stocks of high-end N95 masks were being depleted in stores, with a sales attendant at Changi Airport saying new stocks wouldn't arrive till next week at the earliest. "We've run out of the masks as people going to Europe or the U.S. are trying to resort to some protection from the flu." In Vietnam, there appeared to be a degree of confusion towards swine flu which is not in fact linked to pigs alone -- but an assortment of swine, human and avian viruses. "Death is everyone's destiny but this will be my last pig blood pudding for a while until the flu warning is over," said truck driver Nguyen Huu Luong, as he finished a bright red bowl of fresh pig blood and herbs in downtown Hanoi.
As a whole the nations of Asia were given credit for coming to together quickly to contain the swine flu threat. Health ministers form east Asian countries held meetings after the disease began taking told in Asia. Information was shared. Procedures were transparent. The region seems to have learned lessons after the SARS and bird flu outbreaks. Asian people took matters into their own hands. "I just want to be safe," a Hong Kong man surnamed Cheng told Reuters as he bought 100 child face-masks for his nine-year-old daughter from the Wanchai pharmacy."SARS was like a rehearsal for us," said Wong Pak-keung, a taxi driver who recalled those dark days when streets emptied and few of the city's 7 million people left home without a face mask. "After SARS, people are more prepared and know what to do."
See China, Japan
Image Sources: Wikimedia Commons
Text Sources: New York Times, Washington Post, Los Angeles Times, Times of London, The Guardian, National Geographic, Smithsonian magazine, The New Yorker, Time, Newsweek, Reuters, AP, AFP, Wall Street Journal, The Atlantic Monthly, The Economist, Global Viewpoint (Christian Science Monitor), Foreign Policy, Wikipedia, BBC, CNN, NBC News, Fox News and various books and other publications.
Last updated May 2022
